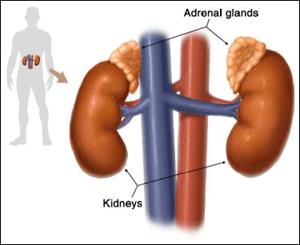
The adrenal glands, located on the top of each kidney, are responsible for releasing different hormones. Adrenal gland disorders occur when the adrenal glands produce too much or too little of these hormones.
The outer part of the gland, called the adrenal cortex, produces the hormones cortisol (pronounced KAWR-tuh-sohl) and aldosterone (pronounced al-DOS-tuh-rohn). The inner part of the gland, called the adrenal medulla (pronounced muh-DUHL-uh), produces the hormones adrenaline and noradrenaline.
These hormones—cortisol, aldosterone, adrenaline, and noradrenaline—control many important functions in the body, including1:
- Maintaining metabolic processes, such as managing blood sugar levels and regulating inflammation
- Regulating the balance of salt and water
- Controlling the "fight or flight" response to stress
- Maintaining pregnancy
- Initiating and controlling sexual maturation during childhood and puberty
The adrenal glands are also an important source of sex steroids, such as estrogen and testosterone.
Adrenal gland disorders occur when the adrenal glands do not work properly. They can be classified into disorders that occur when too much hormone is produced or when too little hormone is produced.
These disorders can occur if there is a problem with the adrenal gland itself, such as a disease, genetic mutation, tumor, or infection. Or, sometimes the disorder results from a problem in another gland, such as the pituitary, which helps to regulate the adrenal gland. In addition, some medications can cause problems with how the adrenal glands function. When the adrenal glands produce too little or too many hormones, or when too many hormones come into the body from an outside source, serious health problems can develop.2,3
Overall, adrenal gland disorders are generally rare. The number of people affected and at risk depends on the specific type of adrenal gland disorder.
Citations
- EndocrineWeb. (2012). An overview of the adrenal glands: Beyond fight or flight. Retrieved May 24, 2016, from http://www.endocrineweb.com/endocrinology/overview-adrenal-glands
- New York Times Health Guide. (2008). Exogenous adrenal insufficiency. Retrieved May 24, 2016, from http://www.nytimes.com/health/guides/disease/exogenous-adrenal-insufficiency/overview.html
- National Library of Medicine. (2013). Adrenal gland disorders. Retrieved May 24, 2016, from http://www.nlm.nih.gov/medlineplus/adrenalglanddisorders.html



 BACK TO TOP
BACK TO TOP