Research
The primary goal of Dr. Sheppard’s translational research group is to develop more efficacious therapies for patients with lymphatic malformations. Specifically, her research has focused on a subtype of complex lymphatic anomaly, called central conducting lymphatic anomaly (also known as channel type lymphatic malformation), with severe morbidity and mortality.
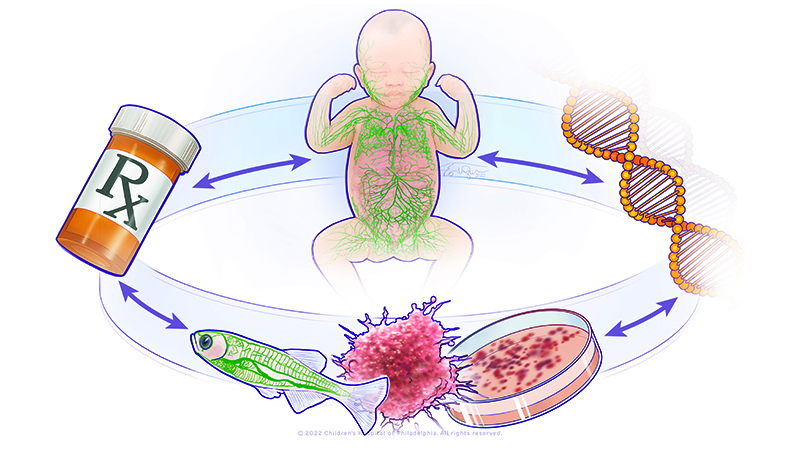
Central conducting lymphatic anomalies (CCLA) occur when there is a disruption of central lymphatic flow resulting in complications such as non-immune fetal hydrops, chylothorax, chylous ascites, protein-losing enteropathy, other effusions, or lymphedema. The heterogeneity of CCLA complicates diagnosis, treatment, and prognostication. Additionally, only about 25% of patients with this disorder have an underlying genetic diagnosis that can be identified. Research from Dr. Sheppard and collaborators identified multiple genetic causes of CCLA and showed that germline RASopathies, mosaic KRASopathies, PIEZO1-related lymphatic dysplasia, and Trisomy 21 all have distinct central lymphatic flow phenotypes. Dr. Sheppard and collaborators also demonstrated that pathogenic mosaic activating variants in KRAS cause CCLA which respond to MEK inhibition in both organoid and zebrafish models.
In her group at NICHD, Dr. Sheppard’s translational research program will have multiple arms. The wet laboratory will elucidate the cellular and molecular mechanisms for known and novel genetic causes of CCLA using organoids and the zebrafish. New therapies will be identified using a drug repurposing strategy. The clinical arm will initially focus on a natural history study for patients with CCLA to understand the disease. This will assist in more efficacious and precise endpoints to study in future clinical trials. A secondary outcome of the natural history study will be to improve molecular diagnosis in patients with CCLA. Eventually, the group will conduct clinical trials from the drugs identified in the laboratory.
The lab is also interested in genetic skin disorders, especially epidermal nevus syndromes and Wiedemann Steiner syndrome. Genetic skin disorders or genodermatoses are genetic disorders with manifestations in the skin, hair, and/or nails. Sometimes patients with epidermal nevus syndromes will have vascular malformations. Wiedemann Steiner syndrome is an autosomal dominant disorder caused by monoallelic (heterozygous) variants in KMT2A. Patients with Wiedemann Steiner syndrome may have developmental delay or intellectual disability, hypertrichosis, constipation, failure to thrive and feeding difficulties, short stature, and vertebral anomalies. Our previous work evaluated 104 participants with WSS from five continents to characterize the clinical presentation.
 BACK TO TOP
BACK TO TOP