Diffuse Optical Brain Imaging
In collaboration with NINDS we have the opportunity to work with two patient groups, each offering a unique opportunity in terms of both patient benefit and scientific research. The first group being war veterans with head injuries where shrapnel is still present in the head. The second study group is children with hemi-spherectomies due to early brain dysfunction. In both cases we aim to study functional behavior in the brain using Near Infrared Spectroscopy (NIRS).
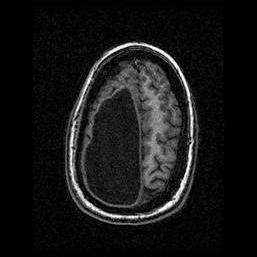
In the first case, the interest is whether in certain key diagnostic areas for brain function we can monitor the veterans as well as we could with fMRI. These patients have suffered traumatic head injury and are in need of careful quantitative monitoring tools. Obviously in the case of the presence of shrapnel we cannot subject the patient to an MRI so an equivalent modality for monitoring structural and functional parameters of the brain is essential. The scientific challenge here will be in studying the effects of the presence of metal in the brain region on optical imaging. The second case is based on a patient group with hemi-spherectomies, composed of children with severe epilepsy or other neurological disorders.
A key area of interest and study for the clinicians here is the evolution of brain plasticity. Moreover, in a fundamental point of view, this work leads to two extremely interesting studies. First, we need to examine the real effect of void regions on reconstruction methods. The second more interesting area is that of being able to determine if we are really seeing activation. Here, uniquely, we can use the empty side of the head as a control, to examine the effects of skin and skull on the depth penetration and signal.
The study has strong clinical interest, first in the usefulness of using NIR technologies in monitoring non-fMRI suitable patient bases, in both study groups. Secondly (and most importantly), the study on hemi-spherectomy patients will also provide useful information on brain plasticity. Here the Clinicians aim to test 4 hypotheses as part of the study:
- Homologous area adaptation, predicts that the homologous area in the unaffected hemisphere can assume a genetically/anatomically predetermined role previously subserved by the lost hemi-sphere.
- Cognitive map change, predicts that there will be a cognitive map change based upon functional experience with implications for surrounding brain areas.
- Compensatory masquerade, predicts that a pre-existing process in the unaffected hemi-sphere can be adapted to a new behavioral role without any plasticity occurring.
- "Limited real-estate," predicts that the remaining hemi-sphere will have to host the array of cognitive processes normally distributed across two hemi-spheres. That will result in the capacity of the hemi-sphere being filled earlier in development than normal with a cost to cognitive processes normally developed late in development (e.g., social cognition).
Our first stage in continuing this project will be to develop our own in-house inverse algorithm. First will be trying to assess numerically the accuracy of geometry in our forward model, and second the inherent problems of meshing complex geometries in 3D. These problems will be assessed using geometries generated from patient CT images. With these we may use our forward model to generate data on exact and perturbed geometries. At this point we may also have to consider that special regularizers or other refinements may be needed for the inverse solver. It is sometimes the case that we may need more sophisticated solvers if our forward problem changes enough to effect the results obtained from an inverse solver, hence developing our own tunable system will be more appropriate than using a closed off the shelf system.
 BACK TO TOP
BACK TO TOP