Credit: Stock Image
View larger image.
Trophoblasts—the outermost fetal cells of the placenta—may be able to contain SARS-CoV-2 and prevent it from spreading to the fetus even though these cells appear to be susceptible to infection by the virus, a study by NIH-funded researchers suggests. Further research into how trophoblasts might contain the virus could lead to ways to prevent COVID-19 in children and adults. The findings may also lead to insights on why fetuses are only rarely infected with SARS-CoV-2.
The study appears in mSphere and was conducted by Yoel Sadovsky, M.D., at the University of Pittsburgh, and colleagues. Funding was provided by NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). Wendy Fitzgerald and Leonid Margolis, Ph.D., of the NICHD Section on Intercellular Interactions, were co-authors of the study.
Background
According to the U.S. Centers for Disease Control and Prevention, roughly 45% of pregnant women with COVID-19 develop symptoms severe enough to require admission to an intensive care unit or ventilator support, or both. Previous studies have found that pregnant women with COVID-19 are more likely to experience pregnancy complications such as preterm delivery.
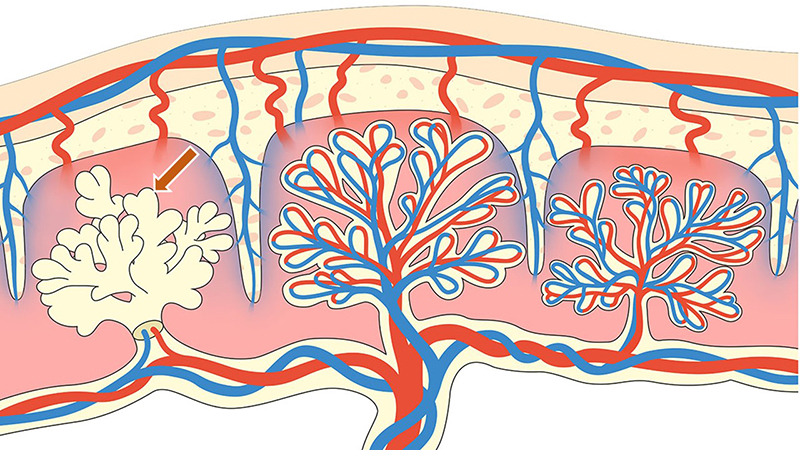
Trophoblasts, the outermost cells of the fetal part of the placenta, come in direct contact with the mother’s blood and are likely to be directly exposed to SARS-CoV-2 circulating in the bloodstream of pregnant women with COVID-19. However, it is rare for a fetus to become infected with the virus. A previous study found that placental cells lack the surface molecules needed for the virus to infect them, but other studies have found that these molecules were present on the surface of trophoblasts and the umbilical cord.
For the current study, the researchers examined trophoblasts and three other placental cell types at or near the surface of the placenta to determine if they had the cell surface molecules needed for SARS-CoV-2 infection. They exposed the cells to pseudoviruses—disabled viruses engineered to have the molecules SARS-CoV-2 uses to enter cells—to see if infection was possible. To infect a cell, SARS-CoV-2 relies on its surface molecule, the spike protein, to bind to ACE-2, a molecule on the target cell’s surface. After the spike protein binds to the cell, the virus commandeers two enzymes on the cell’s surface, TMPRSS2 and furin, to open the spike protein so the virus’ genetic material can enter the cell.
Results
The researchers detected ACE-2 and TMPRSS2 on trophoblasts, but not on the other cell types. All four cell types had furin, with the greatest amount on trophoblasts. Only trophoblasts contained all three molecules.
The researchers also found that pseudoviruses fitted with the spike protein could inject their contents into the trophoblasts. However, antibodies blocking the ACE-2 receptor prevented entry of the viral contents, confirming that the ACE-2 receptor provided the means for the virus to infect the trophoblast.
Significance
Because SARS-CoV-2 is unlikely to infect the placenta and fetus, even though trophoblasts can be infected, the researchers believe trophoblasts may be capable of containing the virus after infection. Research to uncover how trophoblasts may prevent the virus from infecting other types of placental cells may lead to ways to hinder the spread of SARS-CoV-2 in adults and children.
Reference
Ouyang, Y, et al. Term human placental trophoblasts express SARS-CoV-2 entry factors ACE2, TMPRSS2, and Furin. mSphere. 2021.

 BACK TO TOP
BACK TO TOP