Healthcare providers use different tests and measures to diagnose TBI. Often, multiple measures are used together to diagnose TBI and to map out a path for treatment and recovery. Some of these tests are described in the following sections. In addition to “neuro-checks”—a series of quick questions and tasks that help healthcare providers assess how well a TBI patient’s brain and body are working—some in-depth tests help reveal levels of injury or damage in TBI patients.
Please note: This website does not include all tests that may be used to diagnose TBI.
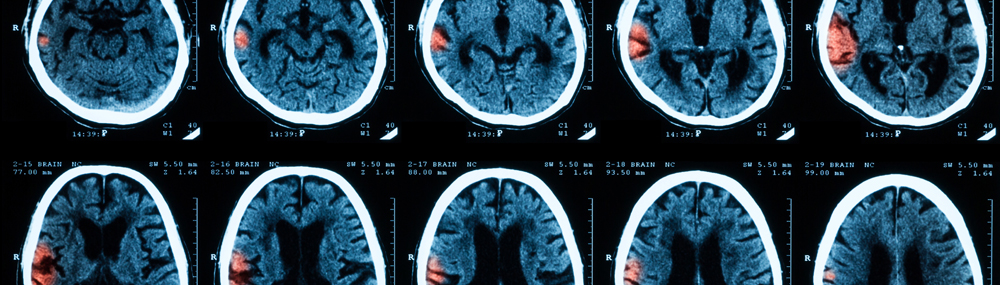
Healthcare providers who suspect TBI will usually take images of a person’s brain. These image tests can include:
- Computerized tomography (CT). A CT (or “CAT”) scan takes X-rays from many angles to create a complete picture of the brain. It can quickly show whether the brain is bleeding or bruised or has other damage.
- Magnetic resonance imaging (MRI). MRI uses magnets and radio waves to produce more detailed images than CT scans. An MRI likely would not be used as part of an initial TBI assessment, because it takes too long to complete. It may be used in follow-up examinations, though.1
The GCS gives healthcare providers a way to measure a person’s functioning in three key areas:
- Ability to speak, such as whether the person speaks normally, speaks in a way that doesn’t make sense, or cannot speak at all
- Ability to open eyes, including whether the person opens his or her eyes only when asked
- Ability to move, ranging from moving one’s arms easily and on purpose to not moving even in response to pain
A healthcare provider rates a person’s responses in these categories and calculates a total score. A score of 13 or higher indicates a mild TBI, 9 through 12 indicates a moderate TBI, and 8 or below indicates severe TBI.2 Doctors can also use the GCS to monitor a patient’s recovery progress.3
Healthcare providers sometimes rank TBI by the person’s level of consciousness, memory loss, and GCS score.
| Mild TBI | Moderate TBI | Severe TBI |
|---|---|---|
| Did not lose consciousness or was unconscious for less than 30 minutes | Unconscious for more than 30 minutes and up to 24 hours | Unconscious for more than 24 hours |
| Memory loss lasted less than 24 hours | Memory loss lasted anywhere from 24 hours to 7 days | Memory loss lasted more than 7 days |
| GCS was 13 to 15 | GCS was 9 to 12 | GCS was 8 or lower.4 |
Other tests for TBI may include:
- Speech and language tests to determine how well the patient can speak and use language, including how well the muscles needed to form words work and how well the patient can read and write5
- Social communication skills tests and role-playing scenarios to determine whether a person’s behavior or actions have been affected
- Tests of swallowing abilities to ensure the patient can swallow safely and receive enough nutrition
- Tests of breathing abilities and lung function to find out whether breathing assistance or extra oxygen is needed
- Cognition tests or questions to see how the patient’s thinking, reasoning, problem-solving, understanding, and remembering abilities are
- Neuropsychological assessments to learn more about the patient’s brain and social functions, including the ability to control one’s behavior and actions
Blood tests to diagnose TBI are an emerging area of research. In 2018, the Food and Drug Administration approved a blood test that detects two proteins, UCH-L1 and GFAP, which are released by the brain into the bloodstream when a mild concussion occurs. The test can help identify individuals whose injury is unlikely to show up on a CT scan, eliminating the need for an unhelpful test. The blood test may also provide a way to quickly diagnose military personnel for a mild concussion.6
Researchers at the National Institute of Nursing Research and NICHD found that testing for the blood protein tau could help identify athletes who need more recovery time before they can safely return to play after a sports-related concussion.7
Citations
Open Citations- Brain Injury Association of America. (n.d.). Diagnosing brain injury. Retrieved March 20, 2020, from https://www.biausa.org/brain-injury/about-brain-injury/diagnosis
- National Institute of Neurological Disorders and Stroke. (2020). Traumatic brain injury: Hope through research. Retrieved March 20, 2020, from https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Hope-Through-Research/Traumatic-Brain-Injury-Hope-Through
- Brain Injury Association of America. (n.d.). About brain injury. Retrieved March 20, 2020, from https://www.biausa.org/brain-injury/about-brain-injury
- Brain Injury Association of America. (n.d.). Glasgow Coma Scale. Retrieved March 20, 2020, from https://www.biausa.org/brain-injury/about-brain-injury/diagnosis/assessments-in-the-hospital/glasgow-coma-scale
- American Speech-Language-Hearing Association. (n.d.). Traumatic brain injury. Retrieved March 20, 2020, from https://www.asha.org/public/speech/disorders/Traumatic-Brain-Injury/
- Food and Drug Administration. (2018). FDA authorizes marketing of first blood test to aid in the evaluation of concussion in adults. Retrieved March 21, 2020, from https://www.fda.gov/news-events/press-announcements/fda-authorizes-marketing-first-blood-test-aid-evaluation-concussion-adults
- National Institutes of Health. (2017). Biomarker in blood may help predict recovery time for sports concussions. Retrieved March 21, 2020, from https://www.nih.gov/news-events/news-releases/biomarker-blood-may-help-predict-recovery-time-sports-concussions

 BACK TO TOP
BACK TO TOP