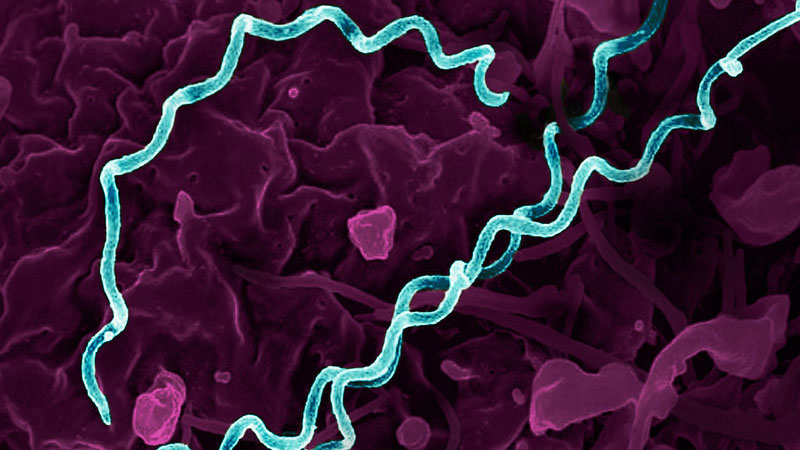
Colorized electron micrograph of Treponema pallidum, the bacterium that causes syphilis.
Credit: NIAID
Although it focuses on celebrating love and romance, Valentine’s Day is also an opportune time to reflect on efforts to enhance sexual and reproductive health by preventing sexually transmitted infections (STIs). In 2022, the most recent year for which data are available, more than 2.5 million cases of the STIs syphilis, gonorrhea, and chlamydia were reported in the United States. The rising rates of syphilis and congenital syphilis are particularly concerning, and are being addressed through a variety of initiatives within the U.S. Department of Health and Human Services.
NICHD supports and conducts a breadth of STI research, with a focus on women, including those who are pregnant, as well as infants, children, and adolescents. Ongoing projects include evaluating a web-based intervention to reduce STIs and substance use during pregnancy and comparing the safety of different antibiotics to treat bacterial infections, including STIs, during pregnancy. We also fund the development and testing of multipurpose prevention technologies—contraceptive products that also protect against STIs—and support a broad range of HIV research, highlights of which are summarized in a recent spotlight on the 35th observance of World AIDS Day.
Addressing STI Prevention Needs for Cisgender Women
Cisgender women have limited biomedical STI prevention options relative to other populations, such as gay, bisexual, and other men who have sex with men and transgender women. One reason for this is that studies of many STI prevention approaches have excluded cisgender women. For example, two daily HIV prevention pills are approved by the U.S. Food and Drug Administration for use by men and transgender women. Yet only one of these medications has been approved for cisgender women, due to a lack of data on the safety and efficacy of the second pill for people who engage in receptive vaginal sex.
Other studies have suggested that STI prevention approaches that work well for men may not translate to women. For example, doxycycline post-exposure prophylaxis (DoxyPEP) is recommended to prevent syphilis, chlamydia, and gonorrhea among men who have sex with men and transgender women. But a recently published study evaluating DoxyPEP among cisgender women in Kenya, funded by NIH’s National Institute of Allergy and Infectious Diseases (NIAID), found that the intervention did not reduce bacterial STIs in this population.
In an accompanying editorial, NIAID Director Jeanne Marrazzo, M.D., M.P.H., discusses the need to consider the biological and behavioral factors that influence STI acquisition in cisgender women when designing biomedical prevention studies. She notes that we need to better understand the science of drug delivery and how it varies between rectal and vaginal tissues. Study designs also should account for the sexual activity preferences of women and common power dynamics with their sexual partners.
Additionally, researchers should consider women’s motivations and contexts for use of a particular product. For example, work supported by NIAID, NICHD, and other NIH institutes led to FDA approval of a safe and effective long-acting injectable form of HIV prevention, offering a discreet option that may be easier and more desirable than a daily pill for some women. Ultimately, we need a variety of tools to prevent HIV and other STIs so that women have multiple options from which to choose.
Curbing the Rise of Congenital Syphilis
An untreated STI during pregnancy can be passed to the fetus or newborn. In the United States, rates of some perinatally acquired STIs, such as HIV, have substantially decreased in recent decades. Unfortunately, rates of syphilis, caused by infection with the bacterium Treponema pallidum, are rising. The rate of syphilis among people giving birth in the United States more than tripled from 2016 to 2022. Syphilis during pregnancy increases the risk of miscarriage, stillbirth, preterm birth, and low birth weight. Infants born with congenital syphilis may experience a range of health issues, including severe anemia, jaundice, and brain and nerve problems.
There were 3,755 reported cases of congenital syphilis in the United States in 2022, reflecting a more than 900% increase in the past decade. As highlighted in a recent review article by NICHD grantee Irene Stafford, M.D., and colleagues, timely diagnosis and treatment could prevent many of these cases and lessen severe outcomes for infants. The authors note that inadequate access to prenatal care often results in lack of timely testing and treatment among pregnant people with syphilis.
Additionally, some babies with congenital syphilis do not show symptoms at birth, and current diagnostic approaches to detect syphilis in these newborns can be inconclusive. New tools that can directly detect T. pallidum infection may lead to prompter treatment for newborns with congenital syphilis and avoid severe complications of the disease. A current NICHD-funded project led by Dr. Stafford is evaluating novel molecular techniques to diagnose congenital syphilis.
To curb the rise in STIs across the nation, we need both new clinical innovations and strategies to optimally implement existing STI prevention and treatment tools. This Valentine’s Day, I encourage everyone to learn more about STIs and NICHD’s research in this area and to consider speaking with your healthcare provider about whether you should be tested for STIs. STI screening is critical for the prevention and management of these infections. HIV.gov offers an online service to find a testing location for HIV and other STIs near you.
 BACK TO TOP
BACK TO TOP