Basic information for topics, such as “What is it?” is available in the About Pheochromocytoma and Paraganglioma section. Answers to other frequently asked questions (FAQs) specific to pheochromocytoma and paraganglioma are in this section.
Pheochromocytoma can be inherited as part of another syndrome or may coexist with other diseases. Some patients with pheochromocytoma have the inheritable disease von Hippel-Lindau (VHL) syndrome or neurofibromatosis type 1 (NF1).1 Both VHL and NF1 are cancer syndromes in which patients have tumors at multiple sites.
Another disease in which pheochromocytoma is often present is multiple endocrine neoplasia type 2 (MEN2), which produces tumors in the endocrine glands, including the parathyroid gland.1 About one half of patients with MEN2 have pheochromocytoma.1
Approximately one third of pheochromocytoma cases are inheritable, and the remaining cases occur sporadically.1 Children are at risk of developing pheochromocytoma/paraganglioma if they inherit one of the known disease-causing mutated genes from their parents. The penetrance of the disease, or the percentage of individuals with a known genetic mutation who develop the disease, varies with different mutations.
Pregnancy may be complicated by the clinical signs of pheochromocytoma. In pregnant people, high blood pressure, cardiovascular problems, and seizures, which occur in patients with pheochromocytoma,2 could affect the health of the unborn child.
Yes. Genetic testing is available for pheochromocytoma. Genetic testing is especially recommended for some groups of patients who1:
- Have a family history of pheochromocytoma
- Have clinical features of syndromes associated with pheochromocytoma
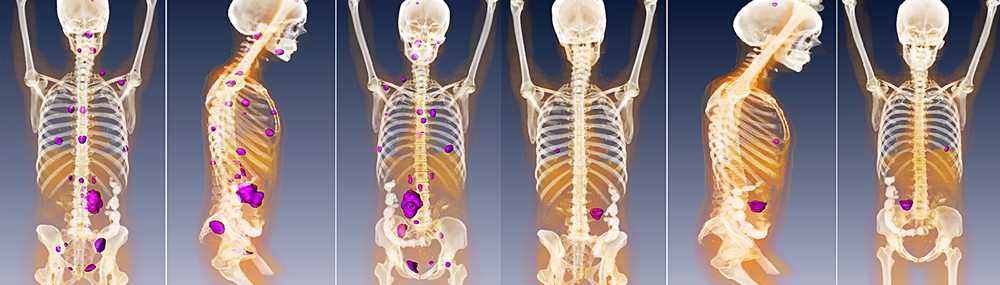
- Have multiple tumors or an extra-adrenal tumor (the tumor is at a location other than the adrenal glands) (paraganglioma)
- Are diagnosed before age 50
- Have specific biochemical results
Genetic testing may also be recommended for other patients, depending upon family history, the patient’s age, and the location of the patient’s tumor.3
Disease screening should be offered to presymptomatic relatives who have a diagnosed mutation, especially because familial syndromes are also associated with other types of tumors and early diagnosis improves the prognosis of these patients. Patients with known genetic mutations should undergo regular periodic screening with biochemical testing and anatomic imaging (CT or MRI scans) to rule out the presence of disease.
Citations
Open Citations- Karasek, D., Shah, U., Frysak, Z., Stratakis, C., Pacak, K. (2013). An update on the genetics of pheochromocytoma. Journal of Human Hypertension, 27(3), 141–147.
- Eunice Kennedy Shriver National Institute of Child Health and Human Development. The proper diagnosis, treatment, genetics, and research of pheochromocytoma and paraganglioma: Overview. Retrieved March 16, 2012, from https://science.nichd.nih.gov/confluence/display/pheo/Overview
- National Cancer Institute. Pheochromocytoma and paraganglioma treatment (PDQ). Retrieved March 7, 2012, from https://www.ncbi.nlm.nih.gov/books/NBK82944/
 BACK TO TOP
BACK TO TOP